
A BRIEF HISTORY OF THE
NATIONAL HEALTH SERVICE (PART 5)
The New NHS: Modern, Dependable
The election of a new Government in May 1997 brought a new approach to the NHS. Pledging itself to abolition of the internal market, the new Government set out an approach which aimed to build on what had worked previously, but discarding what had failed.
Successive Secretaries of State, Frank Dobson, Alan Milburn, John Reid and Patricia Hewitt, would publish a succession of white papers. The initial one was concerned with modifying features of the Conservative reforms that they did not like, for example fund holding. Private practice was first discouraged, and then made an important part a new and more sophisticated market. Later policy documents would feature radical and continuing alterations in structure. Labour's traditional desire to look at health care from a community and public health perspective led it to produce policies on these topics. Alan Milburn and his successors began to encourage patient choice, and to alter financial flows, to try to increase efficiency and flexibility.
But before that, let's go back to that glorious summer of 1997.
Unlike the Thatcher administration of nearly twenty years earlier the new Labour government knew exactly what changes needed to be made to the NHS before they took office. There was to be no honeymoon period, no waiting for the third term before commencing a radical overhaul of the service.
A new white paper issued by the Department of Health on the 9th December 1997, "The New NHS. Modern. Dependable.", put forward a "third way" of running the service - based on partnership and driven by performance. The paper set out an approach which promised to "go with the grain" of efforts by NHS staff to overcome obstacles within the internal market, building on the moves which had already taken place in the NHS to move away from outright competition to a more collaborative approach.
In the foreword to the White Paper, the Prime Minister Tony Blair put forward his vision of the future whilst the subtext reveals a desire to return to the values that had made the Labour party so committed to the NHS some fifty years earlier.
The Government is putting an extra £1.5 billion into the health service during the course of this year and next. More money is going into improving breast cancer and children's services. And new hospitals are being built. The NHS will get better every year so that it once again delivers dependable, high quality care - based on need, not ability to pay.
This White Paper marks a turning point for the NHS. It replaces the internal market with integrated care. We are saving £1 billion of red tape and putting that money into frontline patient care. For the first time the need to ensure that high quality care is spread throughout the service will be taken seriously. National standards of care will be guaranteed. There will be easier and swifter access to the NHS when you need it. Our approach combines efficiency and quality with a belief in fairness and partnership.
As we approach the fiftieth anniversary of the NHS, it is time to reflect on the huge achievements of the NHS. But in a changing world no organisation, however great, can stand still. The NHS needs to modernise in order to meet the demands of today's public. This White Paper begins a process of modernisation. The NHS will start to provide new and better services to the public. For example, a nurse-led helpline to provide advice round the clock. And new technology that links GP surgeries to any specialist centre in the country.
In short, I want the NHS to take a big step forward and become a modern and dependable service that is once more the envy of the world.
By the time the White Paper was published the NHS was spending (or rather consuming) £1,000 a second - the Government wanted to ensure that the money was flowing through the service in a way that ensured both quality and efficiency.
In a clear rebuttal of the methods used under previous administrations Para 9.3 sets out how the new NHS will be an improvement on the 'old.'
The financial regime for NHS Trusts, constructed on a quasi-commercial model, encouraged them to compete for marginal extra income. Health Authorities and GPs, for their part, were expected to attempt to shop around for the 'best buy'. Some family doctors had control over some parts of their budgets but some did not. The result was short-termism that prevented the NHS from planning sensibly for change. Nor did the internal market system prove to be financially disciplined or efficient as record financial deficits and administrative costs both demonstrated.
Six Key Principles
The white paper described this new approach as "a new model for a new century", based on six key principles:
1) To renew the NHS as a genuinely national service, offering fair access to consistently high quality, prompt and accessible services right across the country;
2) To make the delivery of healthcare against these new national standards a matter of local responsibility, with local doctors and nurses in the driving seat in shaping services;
3) To get the NHS to work in partnership, breaking down organisational barriers and forging stronger links with local authorities;
4) To drive efficiency through a more rigorous approach to performance, cutting bureaucracy to maximise every pound spent in the NHS for the care of patients;
5) To shift the focus onto quality of care so that excellence would be guaranteed to all patients, with quality the driving force for decision-making at every level of the service;
6) To rebuild public confidence in the NHS as a public service, accountable to patients, open to the public and shaped by their views.
For the NHS turning 50 rightly meant a celebration, a national recognition of 50 years of healthcare for all - regardless of ability to pay. It also marked the beginning of a new era.
Medical Advances and A New 10 Year Plan
Since the introduction of oral contraception in 1961 attempts had been made to reduce the hazards from thrombo-embolic complications. The hormone content of modern pills was about a sixth of the early preparations, reduction having occurred in stages as new health risks emerged. Progestogen-only pills were also available for women in whom oestrogen was undesirable, as were injectable preparations. In 1995 evidence suggested that two of the newer 'third generation progestogens' were associated with an increased risk of venous thrombo-embolism and the Committee on Safety of Medicines issued a warning. The increased risk, though small, and less than the risk of thrombosis in pregnancy itself, received intense coverage in the media, alarming about half of the 3 million women using oral contraception.
While staff, patients and the public were all encouraged to look back at this phenomenal achievement, the real focus remained on putting into motion the biggest programme of change the NHS had ever seen - a programme which is essentially about putting patients at the centre of the NHS and shifting the focus from a service which does things to and for its patients, to one which works with patients.
But it was only with the publication of the 10 year NHS plan in July 2000 that sweeping plans to transform the NHS into a health service fit for the 21st century came into focus.
The NHS Plan promised:
- More hospitals and beds
- More doctors and nurses
- Much shorter waiting times for hospital and GP appointments.
- Cleaner wards, better food and facilities in hospitals
- Improved care for older people
- Tougher standards for NHS organisations and better rewards for the best
But alongside this, the NHS Plan also promised greater power and more information for patients and the public.
A lot has happened since the NHS Plan was first published, but every development and initiative coming after has its roots in the NHS Plan's core vision of Creating a patient-led NHS.
The NHS in 2005.
This latest chapter in the history of the NHS is still unfolding, but already there are some important milestones which illustrate the scope and the speed of the drive towards patient-centred services:
March 1998 - NHS Direct, the nurse-led health advice service, is launched to give people 24-hour health advice they could trust over the phone. In just five years it grew into possibly the largest single e-health service in the world, handling over half a million calls each month, plus half a million on-line transactions through its web-based service NHS Direct Online. It was the start of a growing range of convenient alternatives to traditional GP services - including the launch of NHS Walk-in Centres, which offer patients treatment and advice for a range of injuries and illnesses without the need to make an appointment.
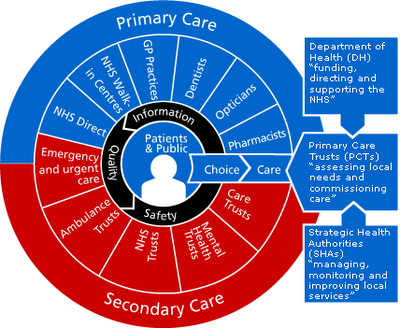
April 2001 - 'Shifting the Balance of Power' was launched to give greater authority and decision making power to patients and frontline staff. The main feature of the change was the creation in 2002 of locally-based Primary Care Trusts - organisations which control 75 per cent of the NHS budget and have the role of running the local NHS and improving the health of people in their areas. At the same time, 28 new Strategic Health Authorities replaced the former Health Authorities and took on a strategic role in improving local health services, while also making sure local NHS organisations are performing well.
October 2003 - consultants in England voted in favour of a new contract aimed at rewarding them more fairly so that more NHS patients benefit from their skills, while also encouraging them to embrace new ways of working in, for instance, multi-disciplinary teams.
April 2004 - new contracts were introduced also for GPs and local family practices, accompanied by new, extra funding for local health services. The new contracts meant, for the first time, all practices are being significantly rewarded for the quality of care they give and not just the numbers of patients they treat.
August 2004 - early patient Choice pilots were extended giving all patients waiting longer than six months for their operation a choice of an alternative place for treatment. This is called 'choice at six months'. By the end of 2005, everyone referred by their doctor for hospital treatment will be offered a choice of at least four hospitals and be able to choose a time that is convenient to them.
Ultimately, by 2008, patients needing planned hospital care will be able to choose to be treated by any healthcare provider in the country which meets NHS standards and NHS prices. As a step towards free choice, from April 2006 patients are able to choose from four or five local providers commissioned by their primary Care Trust, together with all NHS Foundation Trusts and national Independent Sector Treatment Centres.
How Much Does It Cost Me and What Do I Get For My Money?
This is where my professional reputation either sinks or swims with the financial analysis.
Free at the point of service was and has always been one of the factors that has made Britain so proud of its Health Service, but how much does it cost and what do we get for our money?
We pay for the NHS via taxes, the most obvious one being our National Insurance contributions which fund the NHS and our old age pension provisions, I explained the NHS Fund and how it operates in part 2.
A reasonable estimate of the cost would be £62 billion. The current UK population is exactly 60 million which produces an average cost of £1,033. If we multiply £1,033 by the average household size of 2.4 we arrive at a figure of £2,480. This means that the NHS is currently costing the average household about £207 per month, imagine that you could exchange that £207 per month for an NHS Treatment Voucher - what would you get in return?
A heart by-pass operation performed at a private hospital would cost approx. £13,000. So to pay for that you and your wife/husband would have to contribute your £207 a month for five years.
The cost of a single ambulance journey from a hospital/ambulance station to pick-up a patient and take them to A & E is £311 per journey if it is a Paramedic type ambulance - this is based on an average journey time of 49 minutes and includes a provision for abortive trips. The cost of providing a hospital taxi service for elderly or vulnerable patients is £49 per trip.
These figures are based on one paramedic (avg salary £29,030 p.a) and one technician (avg.salary £27,000). The average annual cost per ambulance after taking into account National Insurance contributions is £63,115 p.a per ambulance.
Once you get to hospital the meter is really running:
The cost per bed per day in an intensive care unit is £1,378 or £502,970 per annum
When you get older you actually require less intensive care and so the cost drops to a mere £129 per bed per day - providing of course you are well enough to be looked after on a day ward.
And What Are The Pay Levels Of The Care Providers?
Job: Director of Nursing Annual Salary £50,000
Job: Unit Manager Annual Salary: £24,985 (with 10 years experience)
Job: Specialist ITU Nurse Annual Salary: £19,935
Job: Newly Qualified Nurse Annual Salary: £15,445
Conclusion - Has It Been A Success?
When the NHS was introduced in 1948, it sparked a huge surge of demand for medical care from people who had previously been denied access to free treatment. It is a demand which scarcely seems to have abated since 1948 when hospital waiting lists stood at 500,000. Today the figure is over a million.
On a typical day, 700,000 people visit their GP, but family doctors complain that approximately a quarter of their time is taken up by turgid paperwork, and they do not have the resources to devote proper time to their patients.
In purely medical terms the argument seems overwhelming. Men and women are living about 10 years longer on average than they did in 1948 - men to 74 and women to 79.
And during the last 50 years, medical advances have transformed healthcare, from the invention of a vaccine for polio and the birth control pill in the 1950s to laser and keyhole surgery techniques developed over the last 10 years.
However, nobody could claim that the great experiment has been without its downsides.There have been strikes, health scares, plans, more plans, 10 year plans, pay reviews, GP Charters, Funds etc all in the hope that the NHS that Beveridge visualised in 1941 as being free for all, from cradle to grave, would continue.
Sources:
The most valuable resource is From Cradle to Grave: fifty years of the NHS by G C Rivet ISBN 1-85717-148-9. If I can use an arboreal analogy, this was the trunk which fired my natural inquisitiveness to search for the various branches of the NHS history. Every NHS history online has borrowed from this to a greater or lesser degree, where I have used it, it has been as a starting point.
Other references used:
Historical Background - BBC History - http://www.bbc.co.uk/history/
Comments on the Beveridge Report - http://www.spartacus.schoolnet.co.uk/2WWbeveridgereport.htm
NHS - http://www.nhs.uk
National Audit Office Report: Hip Replacements Getting It Right First Time
is available via http://www.nao.org.uk/
Facts About National Insurance - www.natpencon.org.uk/briefings/b34NInsurance.doc
Advances in Heart Surgery - http://www.bhf.org.uk
Kidney Dialysis - http://www.rds-online.org.uk/pages/page.asp? ToolbarID=3&i_PageID=128
Advances in Clinical neuroscience and rehabilitation http://www.acnr.co.uk/archive.htm
1965 G.P’s Charter - http://www.redbook.i12.com/rb/Docs/rb721.htm
The Beatles Contribute to CT Research http://www.whittington.nhs.uk/default.asp?c=2804&t=1
Minimal Access Surgery - Report 68 Published October 1995 by the Parliamentary Office of Science and Technology http://www.parliament.uk
Developments in British Health Policy - http://www.sun.rhbnc.ac.uk/~uhtm005/nhs.htm
1997 NHS White Paper - The new NHS: Modern Dependable (Cm 3807) is available online at several sites including: http://www.dh.gov.uk/PublicationsAndStatistics/Publications
The 10 Year Plan - http://www.dh.gov.uk/PolicyAndGuidance/fs/en
Personal Social Services Research Unit http://www.pssru.ac.uk/
Nurses Pay Resource : http://www.nursing-pay.com
Modern Britain - A Social History 1750-1985 by Edward Royle published by Arnold
Well that's my homework done, I'm off to watch the Hammers play Palermo!
3 comments:
Wow Paul, i'll give you an A* for that. Do you work as an accountant for the NHS?
Well done Paul. A well written and highly informative set of articles. The explanation of the costs was interesting and it seems we do well for our money. So why do I feel so short changed every time I have an NHS encounter these days?
Due to family circumstances I have regular and frequent contact with GP's, hospitals, consultants etc. I get the feeling that those who are encountered don't really want to be doing the job that they are doing and that we, the users are an irrelevance at best and a nuisance at worst.
Lucy - No I don't work for the NHS although I do have a client who does and I have relatives who did.
Mags - I think there is such low morale in the NHS that you get that attitude sometimes. When I had my angina attack back in July I couldn't have had better treatment and care, cynics might say they were protecting themselves from accusations of poor treatment but all I can say is that they were brilliant and attentive.
Having said that at Doctor level I have a good surgery whilst Janis and Nathalie who are registered with the surgery next door to mine don't get the same attention.
I can't even say its a postcode lottery health service can I?
Post a Comment